

In this blog, IPH Public Health Development Officer, Dr Joanna Purdy, shares insights from a recent seminar on alcohol-related liver disease (ARLD) on the island of Ireland.
In late 2023, the Institute hosted a seminar on alcohol-related liver disease (ARLD) on the island of Ireland on behalf of the North South Alcohol Policy Advisory Group (NSAPAG). The event captured perspectives from public health professionals, clinicians, researchers, advocacy and community sector representatives.

IPH Director of Policy Dr Helen McAvoy chatting with Prof John Ryan and Dr Roger McCorry who took part in the Alcohol-Related Liver Disease seminar.
This blog highlights some of the issues raised during the event, with a focus on the scope for prevention and the health service response.
ARLD in Ireland and Northern Ireland – a snapshot of the data
There can be no doubt that alcohol consumption on the island currently, and over the past 20 to 30 years, is contributing to an increasing burden of alcohol-related liver disease.
Northern Ireland
In Northern Ireland, the number of alcohol-specific deaths[1] have been steadily increasing year on year.
Here are some key statistics and facts to consider:
1 in 50 deaths in Northern Ireland are considered directly attributable to alcohol and it is now evident that alcohol-related liver disease is the main driver of the rising trend of alcohol-specific deaths.
2020 saw the highest ever number of deaths from alcohol-related liver disease and alcohol-specific deaths ever recorded in Northern Ireland.
Alcohol-related liver disease is now the second highest contributor to years of working life lost in Northern Ireland. In other words, this disease kills many people, and does so, at a young age.
The mean age of death from alcohol-related liver disease is just 57 years.
People living in deprived areas are five times more likely to die from this disease than those in non-deprived areas.
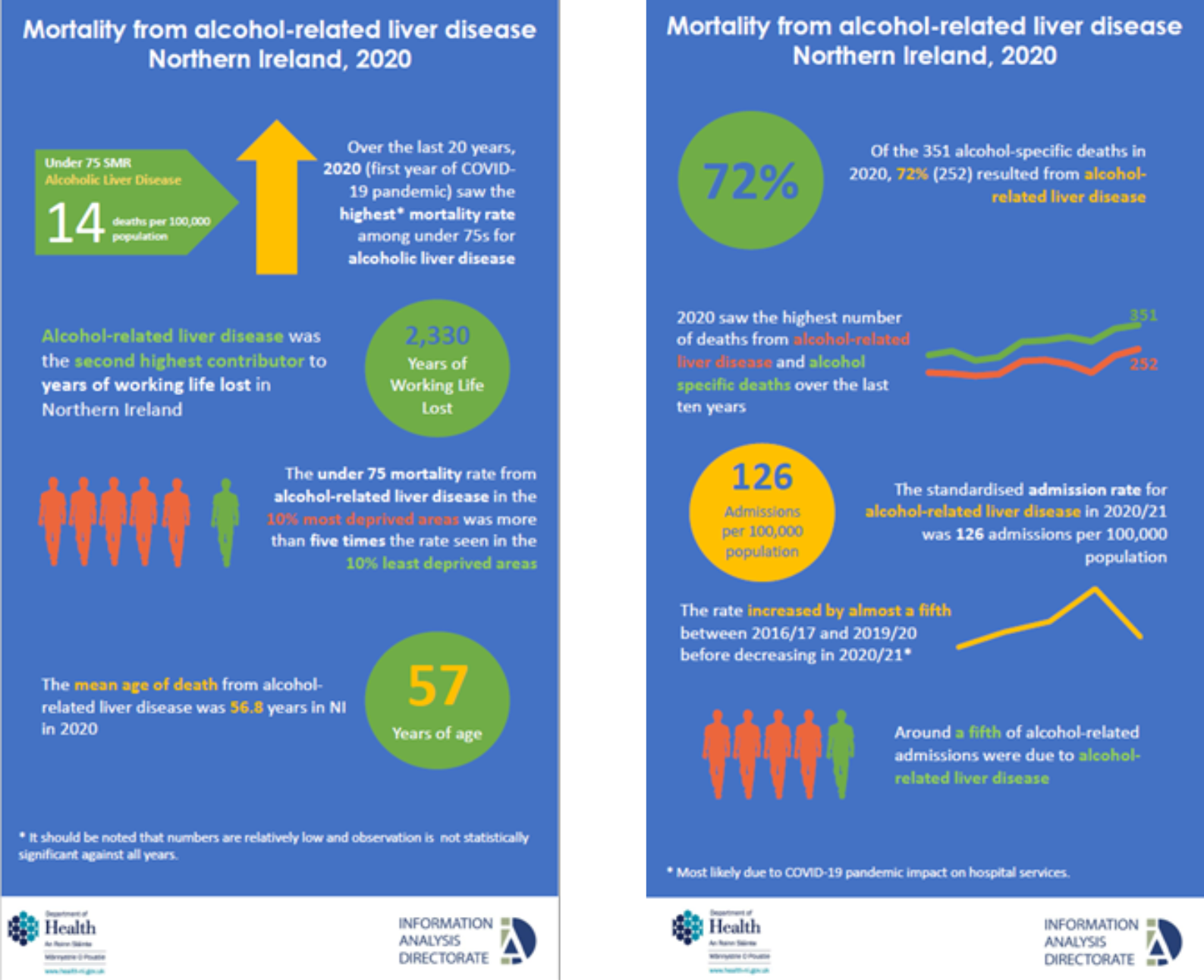
Source: Bill Stewart and Caolan Laverty, Information Analysis Directorate, Department of Health
The NSAPAG seminar heard that the contribution of alcohol-related liver disease to poor population health in the region was under-recognised. Contributors also challenged why the disease receives a fraction of the attention at policy level, and in the media, compared to the other major contributors to early death, like cancer and heart disease.
Ireland
In Ireland the profile of alcohol-related liver disease epidemiology is incomplete due to ongoing deficiencies in health information infrastructure and data collection. The latest available data was presented by Anne Doyle from the Health Research Board.
Here are some statistics and facts to consider:
3,610 hospital discharges were recorded in 2022 with a diagnosis of alcohol-related liver disease.
Across all ages, alcohol-related liver disease discharges increased by 42% between 2001 and 2022, with the highest ever rate reported in 2021.
The data suggests that this form of alcohol-related harm is increasing among both the young and old, with implications for how we perceive risk at community level and within the health service.
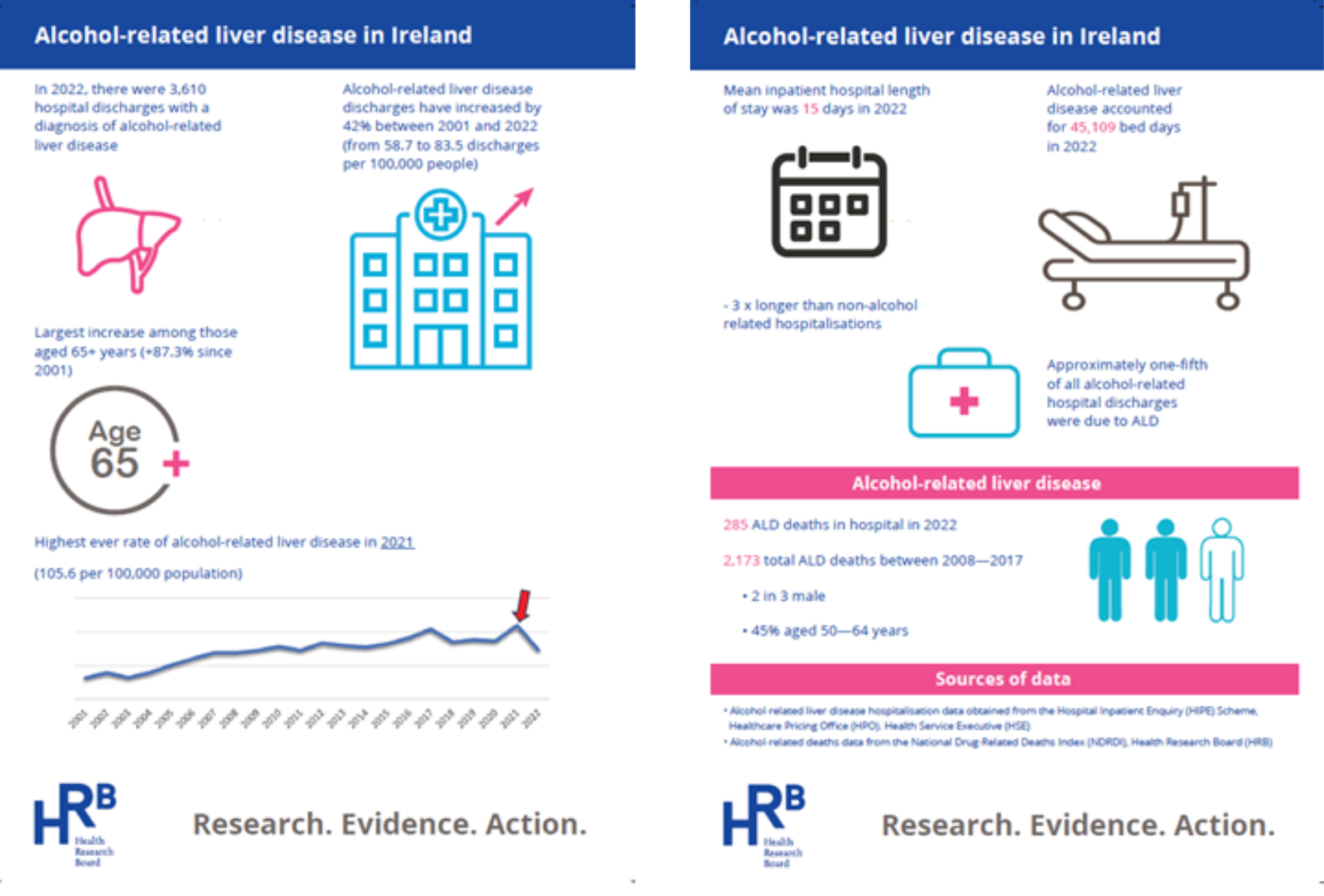
Source: Anne Doyle, Health Research Board
Approaching a policy problem
IPH Director of Policy Dr Helen McAvoy acknowledged the importance of addressing upstream policy on alcohol to ‘turn off the tap’ on the high-risk alcohol use profile of the population. She welcomed the recent establishment of the Irish Liver Foundation and the comprehensive analyses on alcohol-related liver disease presented by the Department of Health in Northern Ireland. While welcoming the Public Health (Alcohol) Act in Ireland she cautioned that a shift in alcohol use at population level will take decades.
In the meantime, there is a rising problem of alcohol-related liver disease, and without a formal response on prevention, early detection, service investment and development and clinical audit, the situation is likely to worsen.
Dr McAvoy further observed that strategies relating to drugs and alcohol in Ireland and Northern Ireland acknowledge the wide range of alcohol-related harms but tend not to specify actions in relation to alcohol-related liver disease. She challenged the audience to consider how we might reframe the response by considering alcohol-related liver disease firstly as a policy failure rather than some sort of ‘failure’ of the individual.
Perspectives from the clinical frontline
Prof John Ryan, a Consultant Hepatologist at Beaumont Hospital, Dublin, and Dr Roger McCorry, a Consultant Hepatologist at the Royal Victoria Hospital, Belfast, shared their experiences of diagnosing and caring for patients with alcohol-related liver disease.
Prof Ryan described admissions to Beaumont Hospital in the previous month noting that 87% of admissions with severe liver disease were alcohol-related. Patients were aged 30-68 years; seven had to undergo emergency procedures; four patients commenced palliative care; and two patients died (aged 41 and 62 years).
Reflecting on his experience, Dr McCorry noted that there is some fatalism, even cynicism, adopted in the response to patients and alcohol-related liver disease is highly stigmatised.
Despite these pre-existing views, the National Confidential Enquiry into Patient Outcome and Death[2] concluded:
not enough was done about the patient’s harmful drinking at the time
there was a failure to screen adequately for harmful use of alcohol
those identified as having alcohol misuse disorders were not referred for support.
So, what can be done to reduce ARLD incidence?
Contributors were supportive of fully implementing all provisions within the Public Health (Alcohol) Act in Ireland and introducing Minimum Unit Pricing (MUP) for alcohol in Northern Ireland as upstream actions to address alcohol-related liver disease.
Early detection and intervention were discussed and both Prof Ryan and Dr McCorry emphasised the importance of a strategic approach to screening for alcohol problems within primary care, the provision of FibroScan technology and appointment of alcohol liaison nurses within appropriately resourced multidisciplinary team. Collectively, these measures can help detect alcohol problems early, allowing for appropriate support and intervention before alcohol misuse leads to alcohol-related liver disease.
Prof Ryan emphasised the return on investment from appointing hospital-based Alcohol Care Teams and multidisciplinary teams.
Dr McCorry noted that modelling studies[3] suggest Alcohol Care Teams in non-specialist acute hospitals will:
save 254,000 bed days annually*
save 78,000 admissions annually*[4]
create a cost saving by the first year of £3.85 for each £1.00 invested.
Prof Ryan further recommended additional recruitment and development of hepatology expertise as this can reduce hospital mortality and readmissions. At present only one in three patients admitted to hospital with alcohol-related liver disease in Ireland were under the care of a liver specialist and this was a contributor to poor outcomes for those patients.
Influencing policy for change
Dr Sheila Gilheany, Chief Executive of Alcohol Action Ireland, called for acceleration on implementation of all provisions within the Public Health Alcohol Act. She proposed a whole of government approach to tackle alcohol-related harm through the establishment of an ‘Office for Alcohol Harm Reduction’ to drive progressive alcohol policy development, coordinate alcohol policy issues across government, commission research to inform policy and set targets for alcohol harm reduction.
Alex Bunting, who is Group Director of Care & Support at Inspire, a mental health and addiction services in Northern Ireland,shared some of the challenges in relation to commissioning and service planning. He proposed that alcohol-related harm should be addressed in the context of poverty and as a priority within approaches to address health inequalities. Mirroring the views of Alcohol Action Ireland, he highlighted the need for policy reform to take on the extent of the problem through a cohesive prevention strategy with cross-departmental alignment. He also referred to the importance of investment in mental health and addiction services coupled with an anti-poverty strategy to target those most in need and most at risk.
Further Information and Resources
If you, or someone you know, is affected by alcohol, the following supports and services are available:
Ireland: Health Service Executive Alcohol Services and Drug and Alcohol Information Support
Northern Ireland: Drugs and Alcohol NI
For more information about Alcohol-Related Liver Disease see:
You can read more about IPH work on alcohol policy here.
References
[1] Prior to 2017 ‘Alcohol Related Deaths’ was used in Northern Ireland and defined as “when the underlying (i.e. primary) cause of death recorded on the death certificate is most directly due to alcohol consumption”. Since 2017, the new definition, ‘Alcohol-Specific Deaths’, includes conditions known to be exclusively caused by alcohol (that is, wholly attributable causes) and excludes conditions where only a proportion of the deaths are caused by alcohol (that is, partially attributable causes). Source: Alcohol-Specific Deaths Northern Ireland Information Paper (NISRA, 2019)
[2] National Confidential Enquiry into Patient Outcome and Death – Alcohol Related Liver Disease: Measuring the Units Report (2013)
[3] Optimal Alcohol Care Teams (ACTs) as part of an effective alcohol treatment system
[4] *by the 3rd year of full optimisation.


