
On World Hypertension Day, Dr Diane Bredin discusses the impact of COVID-19 on hypertension and considers priorities in pandemic recovery. Diane is currently working in general practice and completing an internship with the Institute of Public Health as part of her Masters in Public Health at University of Limerick.
Hypertension is a major preventable risk factor for cardiovascular disease. In Northern Ireland cardiovascular disease is one of the leading causes of mortality, responsible for roughly one quarter of all deaths and claims an average of 10 lives every day.¹ Equally damaging in the Republic of Ireland, it claimed an average of 24 lives daily in 2019.²
Now, more than ever, the health system needs to renew its focus on better prevention and management of hypertension.
Why? Because of evidence on the relationship between hypertension and COVID-19 outcomes, and the ways in which the pandemic has negatively influenced management of the condition. This has occurred through changes in help-seeking behaviours, healthcare delivery and behavioural risk factors.
Impact of hypertension on COVID-19 outcomes
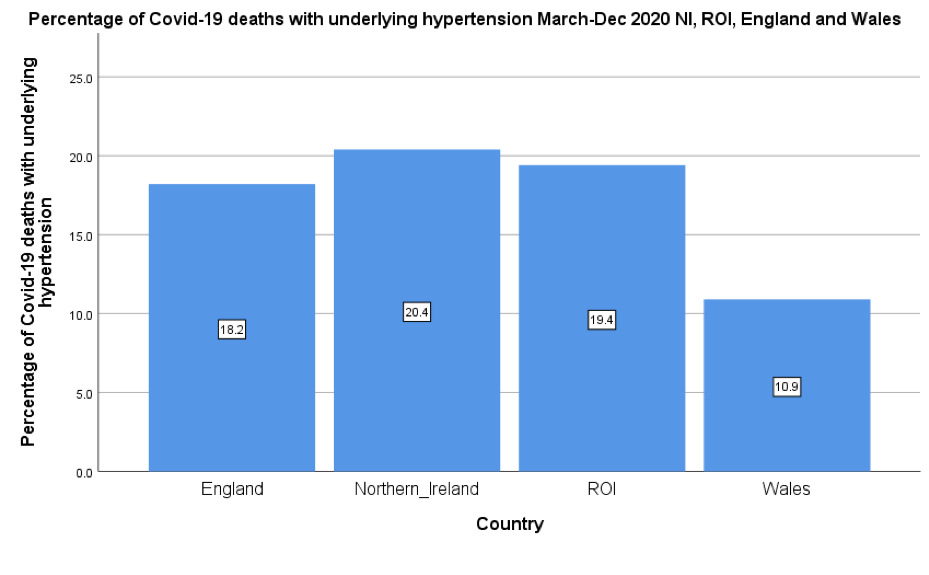
Hypertension has emerged as a common ‘underlying condition’ among people with severe COVID-19 disease and among COVID-19 deaths.⁶·⁷·⁸ Hypertension prevalence increases with age and may be associated with other conditions including obesity, diabetes and cardiovascular disease. The picture is therefore complex, making it difficult to estimate the exact contribution of hypertension alone.
Hypertension was an underlying condition in one in five deaths from COVID-19 on the island of Ireland with prevalence a little higher than England and Wales.
Despite initial concerns, the balance of evidence does not support an increased risk of contracting SARS-CoV-2 or an increased risk of severe disease or mortality amongst patients taking ACEI/ARB medications.⁹
Pandemic impacts on health service use
Globally, most countries have reported disruptions to healthcare services with 53% reporting disruptions to hypertension management and 31% reporting disruptions to cardiovascular emergencies.³
Social distancing measures significantly altered General Practice appointments – in England 40.5% of appointments in February 2021 in England occurred by telephone in comparison to 13.8% in February 2020.⁴
Coupled with health service disruption are changes in help-seeking behaviour. Survey data from Northern Ireland taken between September and January 2021 showed that people were reticent to attend health services – 35% of respondents reported that they would feel uncomfortable (24%) or very uncomfortable (11%) attending A&E for an urgent medical condition.⁵
Pandemic impact on behavioural risk factors
There is some evidence that ‘lockdown’ may have increased behavioural risk factors for hypertension. For some, but not all, there were negative consequences for health behaviours with increases in smoking, poor diet, sedentary lifestyles and increased alcohol use.¹⁰·¹¹
We do not yet fully understand the ‘net impact’ of these behavioural changes at population level, but the evidence to date suggests that the increase in risk factors was concentrated among those with highest risk pre-pandemic. In other words, people living in poverty, with chronic disease and mental ill-health were most likely to experience a worsening of their risk profile.
Now that the wider impact of the COVID-19 pandemic has been considered, the next question is
What considerations must be given to hypertension management in pandemic recovery?
Measure it: Improve hypertension awareness
This year’s theme for World Hypertension Day ‘Measure Your Blood Pressure, Control It, Live Longer’ aims to raise blood pressure awareness.This is an important initial step in reducing cardiovascular disease, as global statistics indicate that 50% of adults with hypertension worldwide are unaware that they have high blood pressure.¹²
Greater awareness is also needed at policy level. An investment in developing more accurate estimates of hypertension prevalence, awareness and control on the island of Ireland would be beneficial in this regard.
Control it: Prioritise the prevention and control of non-communicable diseases including hypertension
Non-communicable diseases (NCDs) are now the leading cause of death in most countries worldwide.³ In 2016, NCDs were estimated to account for 89% of all deaths in the United Kingdom and 91% in the Republic of Ireland.¹³ The disproportionate burden of mortality amongst those with chronic diseases in the COVID-19 pandemic reinforces the urgency to enhance their prevention and management. It is vital that this is prioritized in pandemic recovery in the form of targeted policies and programmes to enhance detection and control of hypertension.
Live Longer: Support healthy living
The benefits of improving blood pressure control on reducing cardiovascular disease are well established. A review in the Lancet found that a 10mmHg reduction in blood pressure reduced the risk of coronary heart disease by 17%, stroke by 27% and heart failure by 28%.¹⁴
Attention must be given to promoting healthier living to improve blood pressure control and for the primary prevention of hypertension. Risk modifying behaviours for hypertension include reducing salt intake, getting regular physical activity, maintaining a healthy weight, eating a healthy diet, moderating alcohol intake and stopping smoking.
Lastly, the pandemic has exposed the extent of health inequalities, with disadvantaged communities carrying a disproportionate burden of COVID-19 disease.¹⁵ This occurred against a backdrop of inequalities in existing non-communicable disease prevalence in these communities.¹⁶
If the aim to ‘achieve better health and wellbeing for everyone’ in pandemic recovery is to be realised, it is vital that we work together to reduce the wider impact of COVID-19, and that we strive to ‘build back better.’
References
1. British Heart Foundation (2017). CVD Statistics- BHF Northern Ireland Factsheet. Available at: bhf-cvd-statistics-northern-ireland-factsheet.pdf
2. Central Statistics Office (2020). Vital Statistics Yearly Summary, 2019. Available at: https://www.cso.ie/en/releasesandpublications/ep/p-vsys/vitalstatisticsyearlysummary2019/
3. World Health Organization and the United Nations Development Programme (2020). Responding to non-communicable diseases during and beyond the COVID-19 pandemic. Geneva. Available at: https://www.who.int/publications/i/item/WHO-2019-nCoV-Non-communicable_diseases-Policy_brief-2020.1
4. NHS Digital (2020). Appointments in General Practice – February 2021. Available at: https://digital.nhs.uk/data-and-information/publications/statistical/appointments-in-general-practice/february-2021
5. Northern Ireland Statistics and Research Agency (2021). Coronavirus (COVID-19) Opinion Survey Key Findings from Phases 1 to 8. Available at: https://www.nisra.gov.uk/sites/nisra.gov.uk/files/publications/NISRA%20COVID-19%20Survey%20Key%20Findings.pdf
6. Health Protection Surveillance Centre (2020). Underlying conditions in confirmed cases of COVID-19 in Ireland, 14 Dec 2020. Available at: Underlying conditions summary_1.0v 14122020.pdf (hpsc.ie)
7. Northern Ireland Statistics and Research Agency (2021). Covid-19 related deaths and pre-existing conditions – March 2020 to February 2021. Available at: https://www.nisra.gov.uk/publications/covid-19-related-deaths-and-pre-existing-conditions-march-2020-february-2021
8. Office for National Statistics (2021). Pre-existing conditions of people who died due to COVID-19, England and Wales. Available here.
9. Lee, M., et al. (2020). Renin-angiotensin system blockers, risk of SARS-CoV-2 infection and outcomes fromCoViD-19: systematic review and meta-analysis. European heart journal. Cardiovascular pharmacotherapy, pvaa138. Advance online publication. https://doi.org/10.1093/ehjcvp/pvaa138
10. Central Statistics Office (2020). Social Impact of COVID-19 Survey November 2020 Well-being and Lifestyle under Level 5 Restrictions. Available at: Introduction and Summary of Results – CSO – Central Statistics Office
11. Sport Ireland (2021). Impact of Covid-19 Restrictions on Sport and Recreational Walking, Q1 2021. Available at: https://www.sportireland.ie/sites/default/files/media/document/2021-05/covid-and-sport-april-2021-q1.pdf
12. World Hypertension League (2021). World Hypertension Day 2021 Fact Sheet. Available at: http://www.whleague.org/images/WHD2021_fact_sheet.pdf
13. World Health Organisation (2018). Noncommunicable diseases country profiles 2018. Available at: https://www.who.int/nmh/countries/en/#U
14. Ettehad, D. et al. (2016). Blood pressure lowering for prevention of cardiovascular disease and death: a systematic review and meta-analysis. Lancet (London, England), 387(10022), 957–967. https://doi.org/10.1016/S0140-6736(15)01225-8
15. Public Health England (2020). Disparities in the risk and outcomes of COVID-19. Available at: https://www.gov.uk/government/publications/covid-19-review-of-disparities-in-risks-and-outcomes
16. Department of Health Northern Ireland (2021). Health Inequalities: Annual Report 2021. Available at: https://www.northernireland.gov.uk/news/health-inequalities-annual-report-2021


